Hallux Rigidus
Fall is upon us here in Anchorage. We hope that you, like us here Alliance Foot and Ankle, have lingering beautiful memories of clear skies, great evenings with friends and family, beautiful mountain vistas, and fish in your freezer. Or maybe your most lingering part of summer is foot pain. If so, we are here to help.
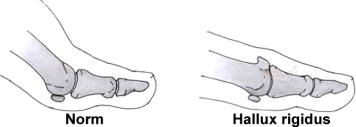
At our practice, we notice that once the weather starts to cool and the days become shorter and our patients find them in our office rather than on the mountain side. One of the more common problems we see with our very active community is pain in the joint of the big toe called hallux rigidus. Common symptoms are pain deep within the joint, a large spur on the top of the joint and decreased range of motion.
This problem usually occurs very gradually. Perhaps you have had occasion discomfort for years or you are just starting to notice a painful bump on your great toe joint. For many people, this can cause significant decrease in doing the recreational activities they love or even difficulty on the job.
What causes it?
There are usually two common causes of hallux rigidus. The first cause is chronic repetitive trauma to the joint that causes a jamming motion such as running, climbing or stubbing your toe can damage the cartilage in the joint. Over time the cartilage may start to erode and your body lays down more bone to protect itself which is what causes the bone spur you may feel at the top or side of the joint.
The second cause is a biomechanical problem related to how the bones in the great toe joint act. The two bones that involved are the first metatarsal (the long narrow bones of the midfoot just behind the toes) and the proximal phalanx (the bone at the base of your great toe). These two bones should line up well allowing the toe to easily glide over the smooth cartilage of the 1st metatarsal. Often times people are born with a slightly more elevated 1st metatarsal. This causes jamming when the great toe attempts to move up and over the head of the metatarsal bone. Over time, this chronic jamming leads to wearing away of the cartilage and extra bone being deposited.

How can it be treated?
Fortunately, we have a variety of ways to treat this condition both from a conservative and surgical approach. The more conservative (non-surgical) approaches involve orthotics that you wear in your shoe to restrict motion of the joint which helps alleviate some of the pain. Icing and anti-inflammatory medications such as Ibuprofen or Naproxen can provide temporary help. Cortisone injections can also be of great benefit in reducing the swelling and discomfort.
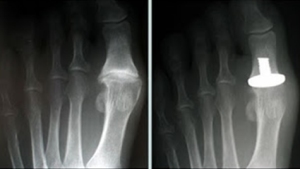
For some people, conservative measures simply aren’t enough. We offer a variety of surgical procedures to correct the issue and return you to your activities. During an office visit, x-rays are taken and reviewed with you by one of our doctors to determine if a surgical procedure is a good fit for you. The procedure chosen is based on the severity of the damage done to the joint, the underlying cause of the hallux rigidus, and the patient’s goals after surgery. Possible procedures are cheilectomy which involves shaving down the painful prominent bone, bone cuts to get correct the alignment of the joint, joint replacement or joint fusion (arthrodesis).
If you think you suffer from hallux rigidus or any other foot problem, we would be happy to help you get back on your feet again.
Dr. Kristin Klingenstein DPM